Article originally published on Healthline
Concerned that the medication she’d taken earlier would wear off during the ceremony, she planned ahead. “I wore a purse under my graduation gown — with a mini water bottle and pill bottle — so I could take my next dose of pain medicine without getting up,” she recalls.
This wasn’t the first or last time she would have to worry about her endometriosis taking center stage. The gynecological condition, which causes tissue from the uterine lining to grow on other organs — is characterized primarily, and explicitly, by pain.
McGaughey, a Wisconsin-based former board member of the Endometriosis Association, has spent several decades managing her agonizing symptoms. She can track hers back to when it began in early adolescence.
“I first suspected something was wrong around age 14 when I seemed to get much more severe menstrual cramps than my friends,” she tells Healthline.
After several years of not finding relief through ibuprofen, however, the doctors she was seeing prescribed hormonal contraceptives to ease her pain. But the pills did no such thing. “Every three months, I was put on a different kind,” recalls McGaughey, 38, who says that some even gave her depression and mood swings.
After many months of not finding a solution, her doctors offered her what felt like an ultimatum: She could continue to be plagued by chronic pain without ever knowing why or go under the knife to find out what was wrong.
While the laparoscopic procedure would be minimally invasive, “The idea of having a surgery just to get diagnosed was hard to swallow as a 16-year-old,” she recalls.
Left with few options, McGaughey eventually chose not to move forward with the surgery. A decision, she says, she would later regret, as it meant several more years spent in severe, undertreated pain.
It wasn’t until after she graduated from college at 21 that she felt mentally prepared to undergo the procedure and finally obtain a diagnosis.
“The surgeon found endometriosis and got rid of as much as possible,” she says. But the procedure wasn’t the cure-all she’d hoped for. “My pain levels dropped significantly after, but year by year the pain returned as the endo grew back.”
For the estimated 1 in 10 women of reproductive age in America affected by the condition, this game of cat and mouse is all too familiar. But unlike other illnesses that have a clear-cut answer, there’s no known cure for endometriosis.
What many of these women are met with, however, is confusion.
When founder and CEO of Flutter Health, Kristy Curry, was in her 20s, she knew something was terribly wrong after nearly passing out in the shower from her menstrual cramps.
Although she was no stranger to long and exceedingly painful periods, this time was different. “I hadn’t been able to make it to work or school for a few days and had been in bed,” recalls the Brooklyn resident. “I thought that was normal as you can’t really ‘compare’ period pain with someone [else].”
All of this soon changed, though, when she found herself headed to the emergency room.
“Women’s reproductive diseases seem to overlap with other issues in the neighborhood,” says Curry, who would go on to have several more years of ER visits for pelvic pain that was misdiagnosed either as IBS or other GI-related issues.
Since endometriosis causes trapped tissue to grow and spread outside of the pelvic region, affected organs such as the ovaries and bowel experience hormonal changes during a woman’s period, causing painful inflammation.
And if your symptoms are complex and take up residence in parts of your body outside of your reproductive system, Curry says, you’ll now deal with even more specialists.
Dispelling misconceptions
The exact causes of endometriosis are still unclear. But one of the earliest theories suggests that it comes down to what’s known as retrograde menstruation — a process that involves menstrual blood flowing back through the fallopian tubes into the pelvic cavity instead of leaving through the vagina.
Though the condition can be managed, one of the most challenging aspects early in the disease is not receiving diagnosis or treatment. There’s also the uncertainty and fear of never finding relief.
According to a recent online survey conducted by HealthyWomen of over 1,000 women and 352 healthcare professionals (HCPs), pain during and between periods are the main symptoms that caused most respondents to visit their HCP to obtain a diagnosis. The second and third reasons included gastrointestinal issues, pain during sex, or painful bowel movements.
The researchers found that while 4 in 5 women who don’t have a diagnosis have indeed heard of endometriosis before, many only have limited knowledge of what these symptoms look like. Most believe the symptoms include pain between and during periods as well as during intercourse. Fewer are familiar with the other symptoms, such as fatigue, gastrointestinal issues, painful urination, and painful bowel movements.
More illuminating, still, is the fact that nearly half of the women without a diagnosis are unaware there’s no cure.
These survey results highlight a major problem concerning the condition. While endometriosis is more widely known than ever, it’s still often misunderstood, even by women have a diagnosis.

A rocky path to diagnosis
One study conducted by a team of researchers in the UK suggests that while several factors may play a role, “one important reason for this disease progression is likely to be the delay in diagnosis.”
Although it’s difficult to determine whether this is due to insufficient medical research, as the symptoms can often mimic other conditions such as ovarian cysts and pelvic inflammatory disease, one thing is clear: Receiving a diagnosis is no small feat.

Philippa Bridge-Cook, PhD, a scientist in Toronto who serves on the board of directors of The Endometriosis Network Canada, remembers being told by her family doctor in her mid-20s that there was no point in pursuing a diagnosis because there was nothing that could be done about endometriosis anyway. “Which isn’t true of course, but I didn’t know that at the time,” Bridge-Cook explains.
This misinformation could account for why nearly half of the undiagnosed women in the HealthyWomen survey were unfamiliar with the methodology of diagnosis.
Later on, after Bridge-Cook experienced several miscarriages, she says four different OB-GYNs told her she couldn’t possibly have the illness, because if she did, she would have infertility. Up until then, Bridge-Cook had been getting pregnant without difficulty.
While it’s true that fertility issues are one of the most severe complications linked to endo, a common misconception is that it will prevent women from conceiving and carrying a baby to term.
Bridge-Cook’s experience reveals not only a lack of awareness on behalf of some HCPs, but also insensitivity regarding the condition.
Considering that out of the 850 survey respondents, only around 37 percent identified themselves as having an endometriosis diagnosis, the question remains: Why is receiving a diagnosis such an arduous path for women?
The answer may simply lie in their gender.
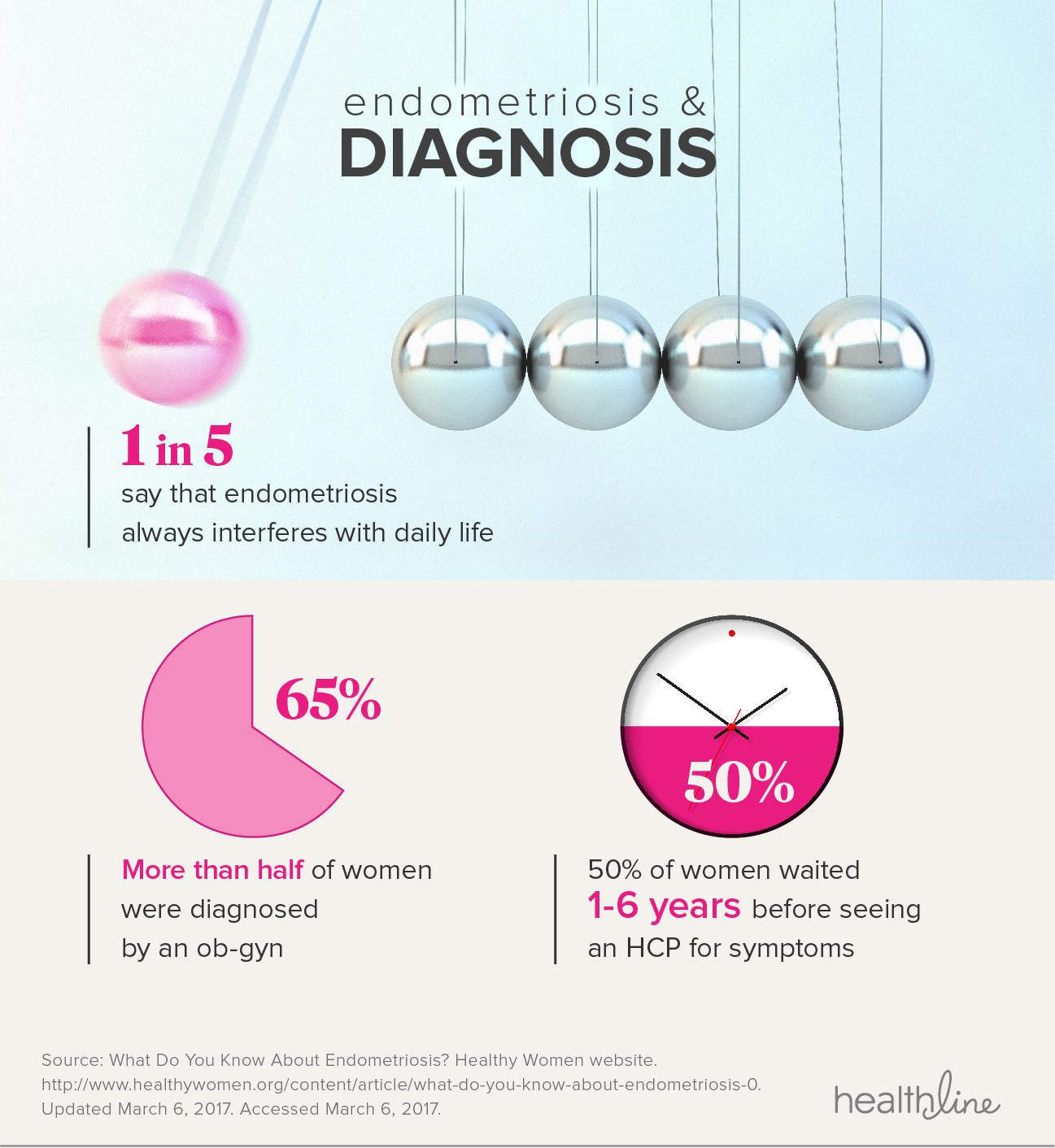
Despite the fact that 1 in 4 women in the survey said that endometriosis frequently interferes with their daily life — with 1 in 5 saying it always does — those that have reported their symptoms to HCPs are often dismissed. The survey also found that 15 percent of women were told “It’s all in your head,” while 1 in 3 were told “It’s normal.” Furthermore, another 1 in 3 were told “It’s part of being a woman,” and 1 in 5 women had to see four to five HCPs before receiving a diagnosis.
This trend is unsurprising given that women’s pain is often ignored or blatantly disregarded in the medical industry. One study found that “In general, women report more severe levels of pain, more frequent incidences of pain, and pain of longer duration than men, but are nonetheless treated for pain less aggressively.”
And it’s often due to this pain bias that many women won’t seek help until their symptoms reach an unbearable degree. Most of the survey respondents waited two to five years before seeing an HCP for symptoms, while 1 in 5 waited for four to six years.
“I hear about many endo patients being prescribed no pain medication,” explains McGaughey, who says she understands that doctors don’t want someone to become dependent on opioids or mess up their liver or stomach with anti-inflammatories. “But this has left many women and girls in extremely severe pain,” she says. “So severe you can’t walk, [with many] thinking they should just take two Advil.”

Research supports her on this — as another study reported that women are less likely to be administered painkillers in the ER, despite acute abdominal pain.
Part of the problem comes down to believing women and girls, McGaughey adds. She remembers telling one doctor that she was experiencing terrible pain with periods, but that didn’t register. Only when she explained that it was causing her to miss multiple days of work each month did the doctor listen and take note.
“From then on, I quantified my pain for professionals in days of missed work,” she says. “That counts more than simply believing my accounts of days of suffering.”
The reasons for dismissing women’s pain are shrouded in cultural gender norms, but also, as the survey reveals, “a general lack of prioritization of endometriosis as an important women’s health issue.”
Life beyond diagnosis
Long after her college graduation, McGaughey says she’s spent an inordinate amount of time tending to her pain. “It’s isolating and depressing and boring.”
She imagines what her life would be like if she didn’t have the illness. “I am so lucky to have my daughter, but I wonder if I’d be willing to try for a second child if I didn’t have endometriosis,” she explains, which delayed pregnancy through years of infertility and culminated in an excision surgery. “[The condition] continues to sap my energy in a way that makes a second child seem unattainable.”

Likewise, Bridge-Cook says that missing out on time with her family when she has too much pain to get out of bed has been the most difficult part of her experience.
Others like Curry claim the greatest struggle has been the confusion and misunderstanding. Still, she expresses appreciation for learning of her condition early on. “I was fortunate, in my twenties, that my first OB-GYN suspected endometriosis and did a laser ablation surgery.” But, she adds, this was an exception to the rule, as most of her HCP’s reactions have been that of misdiagnosis. “I know I lucked out and that most women with endo aren’t so fortunate.”
While the duty of making sure women stay adequately informed about the condition remains on HCPs, McGaughey stresses women should do their own research and advocate for themselves. “If your doctor doesn’t believe you, get a new doctor,” McGaughey says.
Similar to the more than half of survey respondents who were also diagnosed by an OB-GYN, Curry’s endo journey was far from over. Even after receiving a diagnosis and surgery, she went on to spend the next two decades searching for answers and help.
“Many gynecologists aren’t treating endometriosis very effectively,” says Bridge-Cook, who waited 10 years from the time she first suspected something was wrong in her 20s before receiving a diagnosis. “Ablation surgery is associated with a very high rate of recurrence,” she explained, “but excision surgery, which many gynecologists don’t do, is much more effective for long-term relief of symptoms.”
A recent study backs up her up on this, as researchers found a significantly greater improvement in chronic pelvic pain caused by endometriosis as a result of laparoscopic excision when compared with ablation.
According to Bridge-Cook, incorporating a multidisciplinary approach to treatment provides the best results. She’s used a combination of excision surgery, diet, exercise, and pelvic physiotherapy for finding relief. But she also discovered that yoga has been invaluable for managing the stress that comes from living with a chronic illness.
Although McGaughey notes that both her surgeries had the most significant impact on lowering her pain and restoring her quality of life, she’s adamant that no two experiences are the same. “Everyone’s story is different.”
“Not everyone can get high-quality surgeries by surgeons trained to recognize and excise endometriosis,” she explains, and some people are more prone to developing scar tissue than others. Shortening the time to get diagnosed through a nonsurgical method of diagnosis, she adds, could make all the difference.
Advocating for better care
How HCPs treat women experiencing pain is equally, if not more, important to how they address the condition itself. Being conscious of these innate gender biases is the first step, but the next involves having greater awareness and communicating with empathy.
A pivotal breakthrough in Curry’s endo journey arrived soon after meeting a doctor who was not only knowledgeable, but also compassionate. When he began asking her questions unrelated to endometriosis that no other doctor had in 20 years, she started crying. “I felt instant relief and validation.”
While the duty of making sure women stay adequately informed about the condition remains on HCPs, McGaughey stresses women should do their own research and advocate for themselves. She proposes consulting excision surgeons, joining endo associations, and reading books on the subject. “If your doctor doesn’t believe you, get a new doctor,” McGaughey says.
“Don’t wait years in pain like I did out of fear of the diagnostic laparoscopic surgery.” She also recommends that women advocate for the pain treatment they deserve, such as nonaddictive Toradol.
Far from a decades-long quest for answers, these women share an equally ardent desire to empower others. “Speak up about your pain and share all of the nitty-gritty details,” urges Curry. “You need to bring up your bowel movements, painful sex, and bladder problems.”
“The stuff nobody wants to talk about could be key components to your diagnosis and care path,” she adds.
One thing that was made obvious from the HealthyWomen survey is that technology can be a woman’s greatest ally when it comes to staying informed. The results show that most women who aren’t diagnosed want to learn more about endometriosis via email and the internet — and this applies even for those who are diagnosed and are less interested in learning more.
But it can also be used as a means for connecting with others in the endo community.

Despite all the years of frustration and misunderstanding, the one silver lining for Curry has been the women she’s met that’re on the same journey. “They’re supportive and everyone wants to help each other in any way they can.”
“I think now that more people are aware of endometriosis it’s easier to talk about,” Curry says. “Instead of saying you don’t feel well because of ‘lady pain’ you can say ‘I have endometriosis’ and people know.”

Cindy Lamothe is a freelance journalist based in Guatemala. She writes often about the intersections between health, wellness, and the science of human behavior. She’s written for The Atlantic, New York Magazine, Teen Vogue, Quartz, The Washington Post, and many more. Find her at cindylamothe.com.

 Copyright secured by Digiprove © 2018 Linda Girgis, MD, FAAFP
Copyright secured by Digiprove © 2018 Linda Girgis, MD, FAAFP