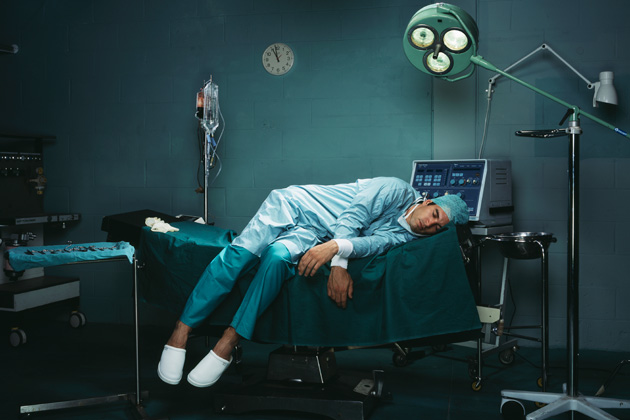
Burnout definition: “physical or mental collapse caused by overwork or stress”
Many doctors are always a step away from burnout. Doctors are expected to keep long hours and always be available. Life saving decisions often need to be made in seconds. And if we fail, people can die. Yet, knowing this, we all chose this profession anyway because we want to make a difference
Burnout rates are escalating among physicians, as well as other healthcare workers. In a system that is already stressed by many forces, losing any member of the team can have devastating consequences. Nurses are a prime example of how they are expected to do more and more work with less and less help and resources. Hospitals cut back on their ranks to save money. And patients suffer because of it. Big organizations do not so much care about the health of these nurses who selflessly try to give patients their best. Rather, the bottom line dictates staffing standards.
Factors causing burnout among doctors:
- Mindless bureaucracy. We see the patient and discuss their care with them. It is agreed upon the best next course of action. The test gets ordered and then the doctor and his staff gets thrown into prior-authorization purgatory. While the fires are heating up. the patient keeps calling to find out the status on authorization. Yet, no one has an answer to give because the insurance company is reviewing the medical necessity of the test for days. This is enough to drive one patient mad. imagine doing this same scenario many times a day, day after day. Doctors just want to practice medicine.We don’t want to play insurance company roulette.
- Needless regulations. Many people see the need for electronic health records and better management of patient data. But then the government stepped in and regulated how we record that data. Seeing a patient is now a data-recording feat that must comply with rules set up by the government who does not understand how these things work. We saw how meaningful use caused havoc on many practices and organizations. Yet, when the government realized they weren’t able to enforce Stage 3 because the technology still was not able to do a key goal of the HITECH Act (ie interoperability), they bailed out of the program and revamped it. Now we have MIPS/MACRA which increases are data work-load further while threatening our payments at the same time.
- Unrealistic expectations from patients. Everyone needs a break sometimes. Yet, when I return from an infrequent vacation, there are some patients who rain down their ire on me for being away when they needed me. this despite the fact that we pay another physician to cover the practice when we are away. Patients expect good outcomes with no side effects. It just doesn’t work that way and no matter how much pressure is placed on us, we cannot deliver the impossible. Sometimes bad things happen which are unpreventable.
- Increasing overhead costs with stagnate or dwindling reimbursements. I haven’t had a raise in reimbursements since I started practicing 17 years ago. Yet, my rent and many other costs rise yearly. Small practices are struggling to stay solvent. Yet, many people still label us as greedy.
- Increasing medical knowledge. Medical knowledge advances at rapid-fire speed. It is the responsibility of doctors to keep abreast of all the latest medical information.
- Top-heavy executives. Many healthcare executives are businessmen/women without any medical background. There are more of them than ever before. If you can think of a department to create, you can probably find 2 or 3 vice-presidents to be in charge of it. They rule the roost and for the most part, their success is tied to finances. Doctors are expected to make money. Doesn’t matter if you are a skilled doctor or have a good bedside manner, you need to make that cog in the wheel flow quickly and bring in top dollars.
- Voicelessness. Most can agree that our healthcare system has grown quite dysfunctional. For years, doctors were prohibited from joining together to fight the injustices in the system that we work in. It is illegal for us to form unions or collectively bargain. For doctors who speak out, they often get labeled as disruptive and their jobs threatened. Additionally, many of the organizations that we trusted to represent our interests failed us. Everyone knows the AMA and think it speaks for doctors. yet, only 18% of doctors remain members because we do not feel they have our interests at heart. Rather, they have joined the political arena and left us to fend for ourselves.
Doctors are facing pressures like never before on many fronts. We are working long hours with little time off and more and more is expected from us. We are no longer a respected profession and have little voice left in our sector. No wonder burnout is becoming the norm.
Photo credit: Bloomberg
 Copyright secured by Digiprove © 2017 Linda Girgis, MD, FAAFP
Copyright secured by Digiprove © 2017 Linda Girgis, MD, FAAFP